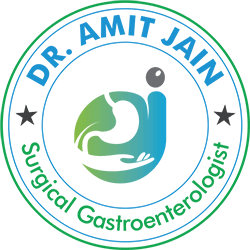
Pancreas Anatomy
Pancreas is a retroperitoneal organ, divided into head, body and tail. It lies posterior to the stomach. The head part is surrounded by the duodenum and distal part of the common bile duct (CBD) passes through this part. Tumor located in this part causes duodenal and CBD obstruction leading to vomitting and jaundice respectively
Pancreatic juice is secreted into the pancreatic duct, Near the duodenum this duct joins with the terminal part of CBD and form a common channel called as ampulla of vater. Periampullary cancer include carcinoma of head of pancreas, distal CBD and duodenum near ampulla of vater
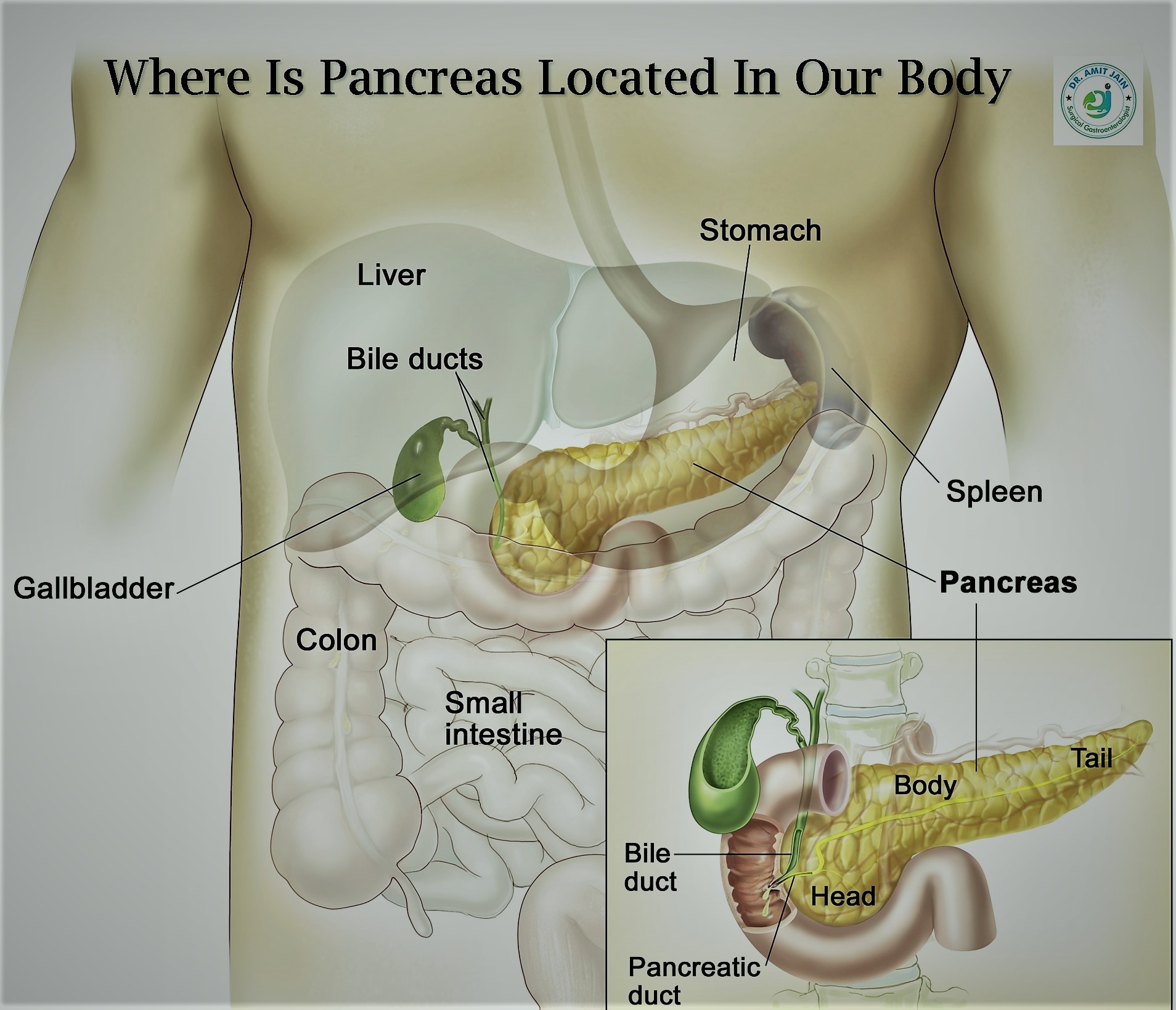
Pancreas Function
The pancreas has got dual function, exocrine & endocrine.
The exocrine function means pancreas releases digestive enzymes which help in digestion. The main digestive enzyme released is amylase and lipase, helping in fat digestion. This is the reason fat digestion is first and most commonly affected in pancreatic disorders
The endocrine function include synthesis of hormones which mainly regulate carbohydrate levels in our body. the main include insulin & gulcagon. Pancreatic disease patients are prone to develop diabetes mellitus and hypoglycemia
Acute Pancreatitis
Inflammation of pancreas is acute pancreatitis, most common pancreatic disorder .There are two main reasons one is Alcohol intake and other is Gallstone, Diagnosis is based on increased serum amylase and lipase level and the typical pain abdomen localized to epigastric region and radiating to back; CECT abdomen is done after 72 hrs of onset of pain abdomen to assess the severity of acute pancreatitis.
The course of disease is counted from the day of onset of pain abdomen, Organ failure in the first 72 hr carry a bad prognosis and high mortality rate; Initial phase is body inflammatory response to pancreatitis and can last up to 2-3 weeks, during this phase chances of pancreatic infection is less; After 4th week patient can develop pancreatic abscess and later on acute fluid collection may organize to pseudocyst.
First 2-3 weeks patient require critical care; Respiratory and Inotropic supports if required, Enteral nutrition should be started as early as possible; If patient does not tolerate enteral feed because of gastroparesis, a naso-jejunal tube can be placed by gastroenterologist.
Most common indication of surgery in these patients is infected pancreatic necrosis or pancreatic abscess. Pancreatic necrosectomy is done either by open or laparoscopy approach
Team approach is required for the best outcome of these patients. In the initial or inflammatory phase critical care specialist role is utmost. Intra-abdominal collections may require drainage under USG or CT guidance by intervention radiologist doctor. GI surgeon has to take decision about the need and timing of surgical intervention.

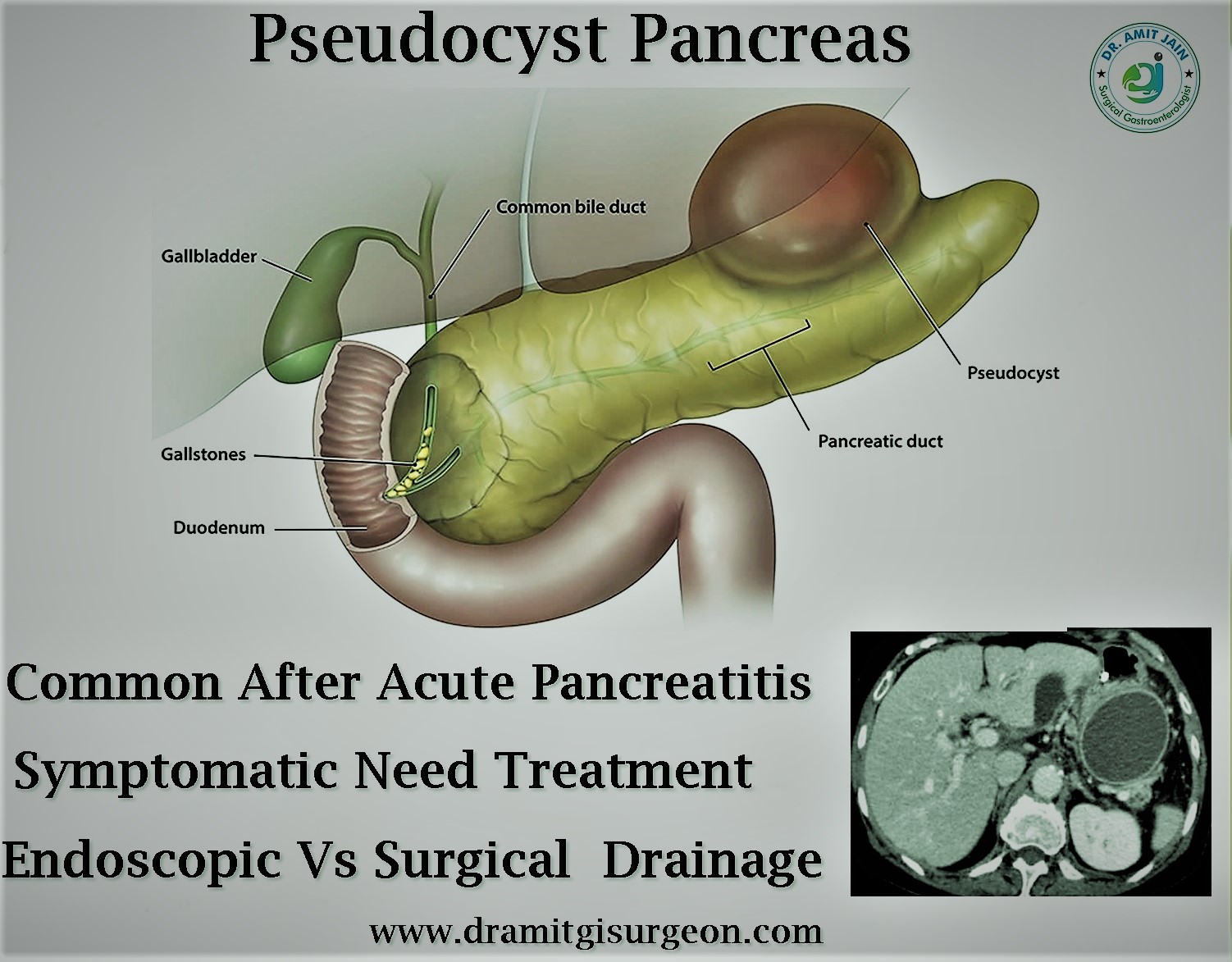
Pseudocyst Pancreas
After an episode of acute pancreatitis if peri-pancreatic fluid collection does not resolve then after four weeks these are termed as pseudocyst
Not all pseudocyst require intervention because many of these pseudocyst remain stable or regress; however cyst which are increasing in size and causing pressure symptoms or develop complication require intervention
As many of these pseudocyst communicate with pancreatic duct, simple external drainage is not effective, these require some type of internal drainage into bowel; which can be done either by endoscopy or surgical intervention; MRI abdomen will tell whether the contents of the cyst are liquefied or solid, because if the contents are solid endoscopy drainage will not be success; Surgical intervention are cysto-gastrostomy or cysto-jejunostomy depending on location. Most commonly these are retro-gastric and bulge into the stomach and cysto-gastrostomy is the procedure of choice. These procedures are done mostly by laparoscopy approach with minimal incision
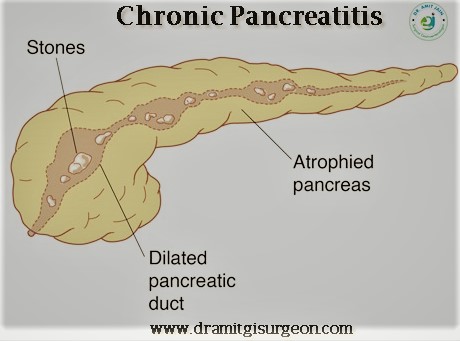
Chronic Pancreatitis
Alcohol intake is the most common cause of chronic pancreatitis. Repeated inflammation of the pancreas due to alcohol leads to pancreas atrophy and loss of pancreatic function
Pancreatic duct dilatation due to pancreas atrophy, calcification’s, ductal stones are hallmarks of chronic pancreatitis
Patient complain of severe pain abdomen which become constant requiring frequent hospital admissions. These patients become narcotic drugs dependent, because of severe pain
Loss of pancreatic function leads to diabetes and steatorrhea. Steatorrhea is passing undigested fat in the stool. The stools are typically bulky, frothy and difficult to flush. It is an indication for pancreatic enzymes supplementation
Most of these patients are managed medically with symptomatic treatment. Refractory pain is indication of surgery. The theory behind severe pain in chronic pancreatitis is pancreatic duct hypertension and idea of surgery is release of pressure in the pancreatic duct. It is done by laterally opening the pancreatic duct and drain into jejunum. Pancreatic head is said to be epicenter of pain origin and simultaneously head coring is done
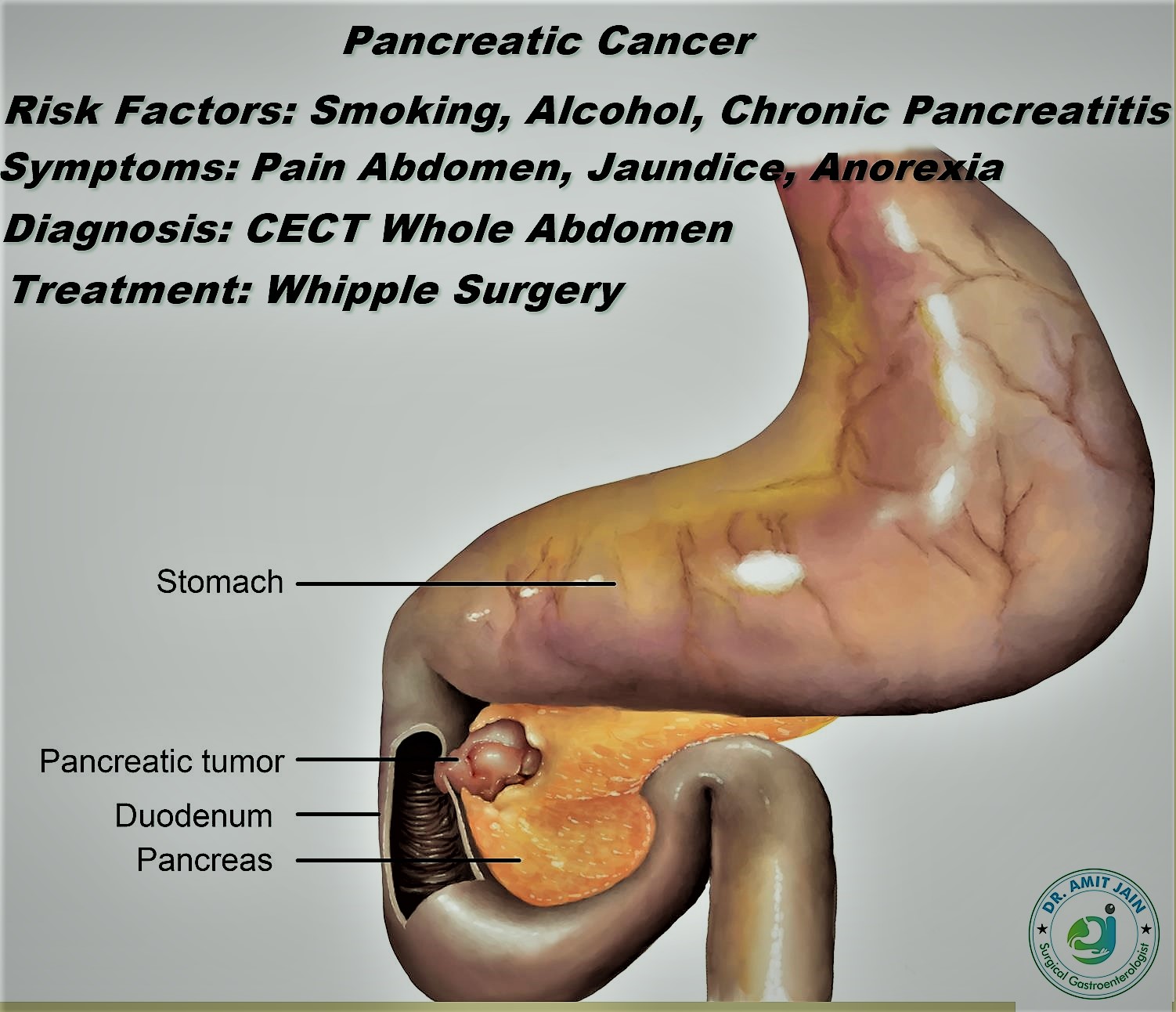
Pancreatic Head Cancer
Risk factors for pancreatic cancer include smoking, alcohol, chronic pancreatitis
Pancreas is divided into three parts head, neck and body region. Symptoms depend at the site of tumor location, if the cancer is located in the head region, patient present with jaundice/vomiting and if in neck and body region pain and abdomen mass as the main symptom; weight loss and decreased appetite are common symptom
CECT abdomen is done which show any local and distant spread; Tumor is said to be locally advanced when it involves surrounding major vessels which include superior mesenteric vein (SMV) and portal vein (PV). In these patients pre-operative chemotherapy is given to down stage the tumor. Involvement of superior mesenteric artery (SMA) more than 180 degree generally precludes any surgical intervention
If the tumor is resectable and located in the head region, the standard surgical procedure is Whipple procedure (Pancreatico-duodenectomy); and if the tumor is located in body and tail region the standard surgical procedure is distal pancreatectomy with splenectomy
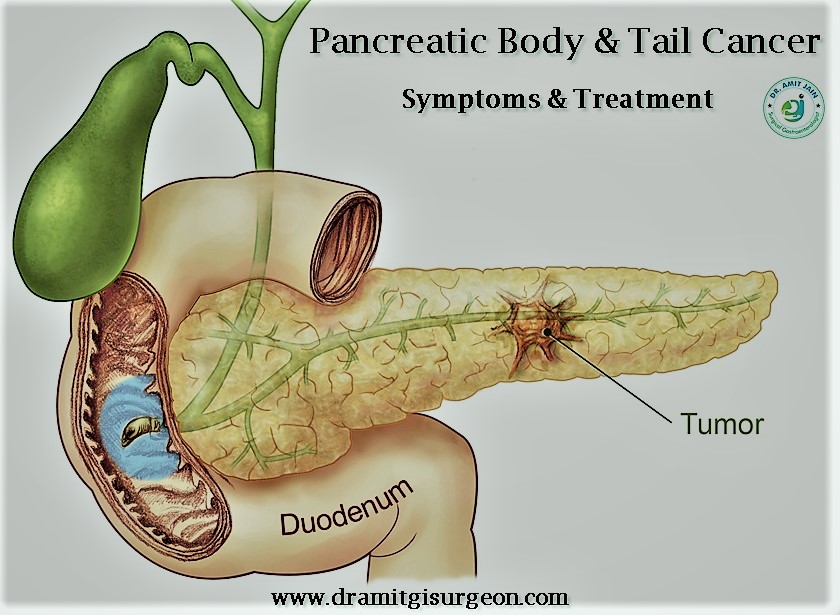
Pancreas Body & Tail Cancer
The incidence of cancer in the pancreatic body & tail is less as compare to head malignancy. Because of the location,these tumors grow to big size before they become symptomatic.
Most commonly patient present with pain abdomen or lump abdomen, when investigated for these symptoms are diagnosed to have pancreatic cancer
PET Scan can be done in these patients as the chances of metastases are high in these patients.
Before proceeding for definitive resection, staging laparoscopy is must for these cancer. It can detect missed metastatic lesions on PET scan and further as these patients does not require any palliative by-pass procedure, it can avoid the pain and morbidity of long incision
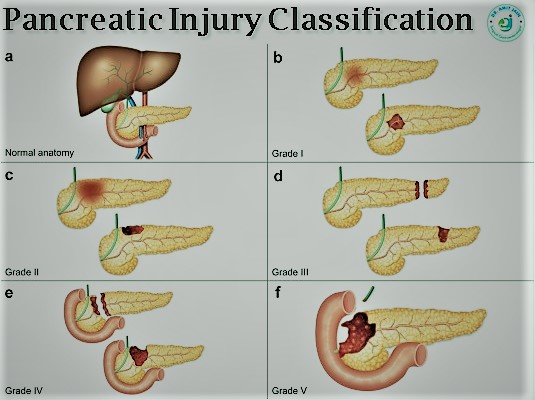
Pancreatic Injury
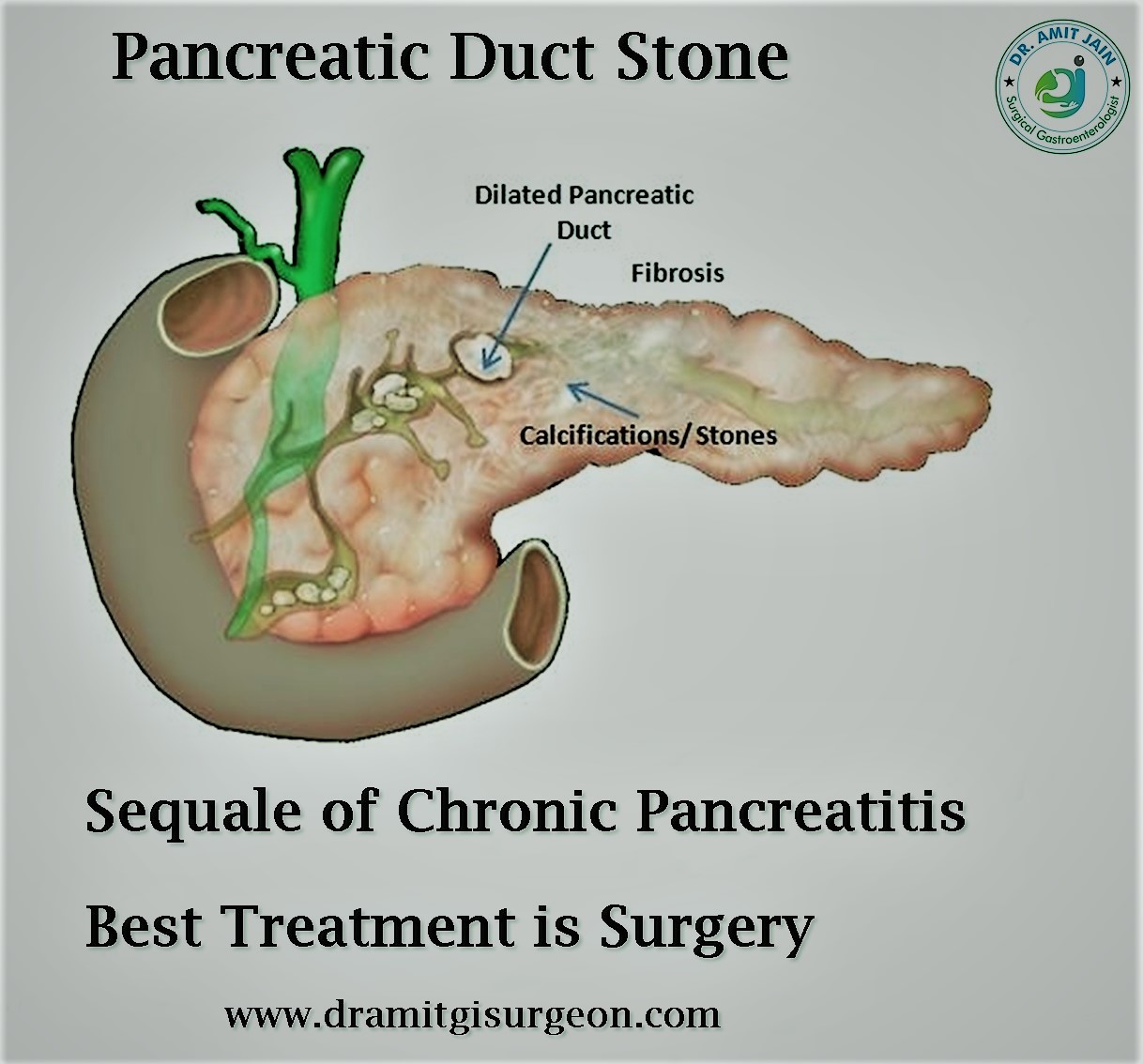
Pancreatic Duct Stone
Pancreatolithiasis, or pancreatic calculi (PC), is the end result of chronic pancreatitis (CP) irrespective of the cause. Stones may occur in the main ducts, side branches or parenchyma. Generally contains a nidus over which there is deposition of calcium carbonate layers
The stones causes obstruction in the main pancreatic duct resulting in ductal hypertension. Pain is the cardinal symptom and occur due to ductal hypertension
Treatment of choice for small calculi is endoscopic retrograde cholangiopancreatography (ERCP) followed by sphincterotomy and extraction .Fragmentation by extracorporeal shock wave lithotripsy (ESWL) may be required for large stones prior to their extraction or spontaneous expulsion. Endotherapy is useful when there is no associated pancreatic duct stricture
Surgery is best options in patients who have extensive stones, ductal strictures and when endoscopic therapy fails
Laparoscopic Pancreatic Surgery
Pancreatic surgery are complex major abdominal surgeries. Experience and skills determine the outcome. Most of these surgeries are performed by open approach. But with the advancement in the Laparoscopy techniques and instruments, Nowadays most surgery can be performed by this minimally invasive approach by trained GI Surgeon or Laparoscopic Surgeon or Pancreatic surgeon
Most commonly surgery performed Laparoscopy are pancreatic necrosectomy and internal pseudocyst drainage which develop after an episode of acute pancreatitis. Pancreatico-jejunostomy for chronic pancreatitis
Whipple procedure is done most commonly by open approach , but some advance laparoscopic centres in the world are doing this complex surgery Laparoscopy


Pancreatic Surgery Cost
Pancreatic surgery are major and complex GI surgery. GI or Gastrointestinal Surgeon are competent and experienced surgeon for such surgeries. Tertiary care level hospitals are best as these have all the infrastructures needed
The cost of surgery depends on the indication of surgery and patient general health status. Patients of acute pancreatitis with pancreatic necrosis are sick patients and may require prolong ICU & hospital stay, which may cost more, rather than surgery itself
Laparoscopic procedures cost more as compared to open
Keep Your Pancreas Healthy. Know How?
 Avoid Alcohol, Known cause of Pancreas inflammation (Pancreatitis) & Cancer of the pancreas
Avoid Alcohol, Known cause of Pancreas inflammation (Pancreatitis) & Cancer of the pancreas
Stop Tobacco
Healthy pancreas diet should be rich in protein and low in fat
Do regular exercise and maintain weight
Get rid of gallbladder if it has stones