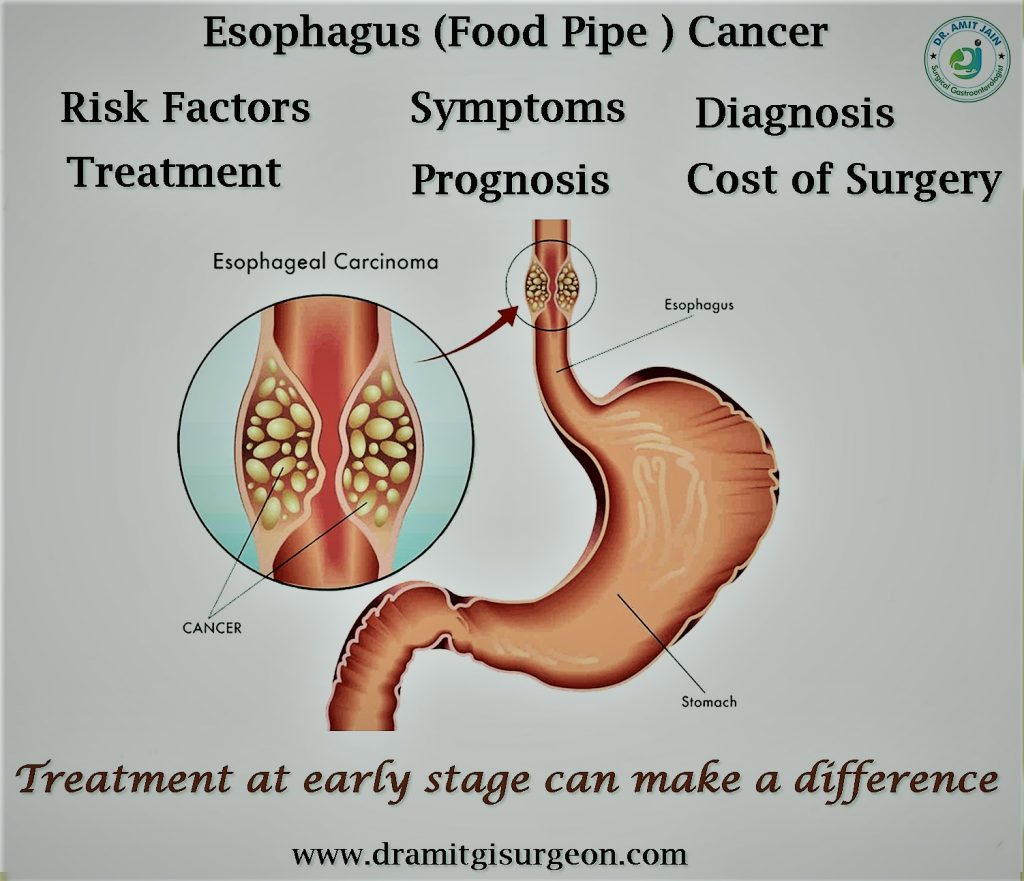
Cancer Oesophagus
Smoking, alcohol intake, obesity and GERD are common Oesophagus cancer risk factor. Smoking and alcohol cause squamous cell carcinoma. Obesity and acid reflux are risk factors for adenocarcinoma. Healthy life style can prevent esophagus carcinoma The most common symptom is dysphagia. Initially it is for solid food and gradually to liquid also. Patient can have chest pain/regurgitation. Anorexia and weight loss are common. Advance carcinoma patients can have bony pain, abdomen distension due to ascites, respiratory distress due to pulmonary effusion.Diagnosis: Upper GI Endoscopy is done by gastroenterologist and is the investigation of choice. It will show growth or stricture in the esophagus. Biopsy will confirm the diagnosis. Most common type of esophagus carcinoma is adenocarcinoma located in the lower third of esophagus. Squamous cell carcinoma is other type and mainly found in the upper and middle third of esophagus
Investigations: CECT Chest and upper abdomen is done.CECT will show the growth in the esophagus, its relation with surrounding structures, any associated lymph nodes, and metastases. It helps in planning of Oesophagus carcinoma treatment. PET scan is done in selective patients who have bulky and long tumor and in high risk patients for surgery. The purpose is to identify distant metastases missed on CT scan
Treatment The recommended first line Esophagus Cancer Treatment is surgery if cancer is resectable. For locally advance tumor pre-operative chemo-radiotherapy is given.If patient respond to chemotherapy and tumor become resectable surgery is done. For metastatic disease endoscopic esophageal stent is placed for relief of dysphagia. If endoscopic stenting is not possible feeding jejunostomy is done surgically for nutrition
GERD : Common Oesophageal Disease
Gastroesophageal reflux disease (GERD) as the name indicates is the reflux of stomach contents back into the esophagus. Generally what happens, when we ingest food it passes through the esophagus, there is a valve at the lower end of esophagus which relax or opens and food enter into the stomach and after that valve gets closed. When this valve is not competent enough stomach contents reflux back.Causes Improper function of lower esophageal sphincter muscle as described above is the reason for gastroesophageal reflux
Symptoms: Heartburn (Burning sensation in chest, usually after eating, worsened at night) Regurgitation of food contents Difficulty swallowing Chronic cough/ New or worsening asthma
Risk Factors : Obesity, Hiatus Hernia, Delayed stomach emptying, Pregnancy Smoking, Alcohol/ Coffee, Eating large meal
Complications: Esophagus ulcer is the first finding on endoscopy in simple reflux disease. Long standing reflux can cause Barretts esophagus which is a premaligant condition which predispose to esophagus cancer. Continuous reflux can cause benign esophageal stricture
Diagnosis: Oesophageal pH monitoring is the gold standard test to confirm the prsence of reflux Upper GI Endoscopy Esophageal Manometry
Treatment First step is life-style modification Medical treatment include proton pump inhibitors which decrease the amount of acid produced by the stomach. these includes pantocid, rabeprazole. Another group of medicines which are beneficial include H2 blockers, Antacids, Prokinetics Surgical management: Surgery is indicated if above methods fail, and lower esophageal sphincter muscle is weak, associated hiatus hernia. In these cases Niissen fundoplication is done
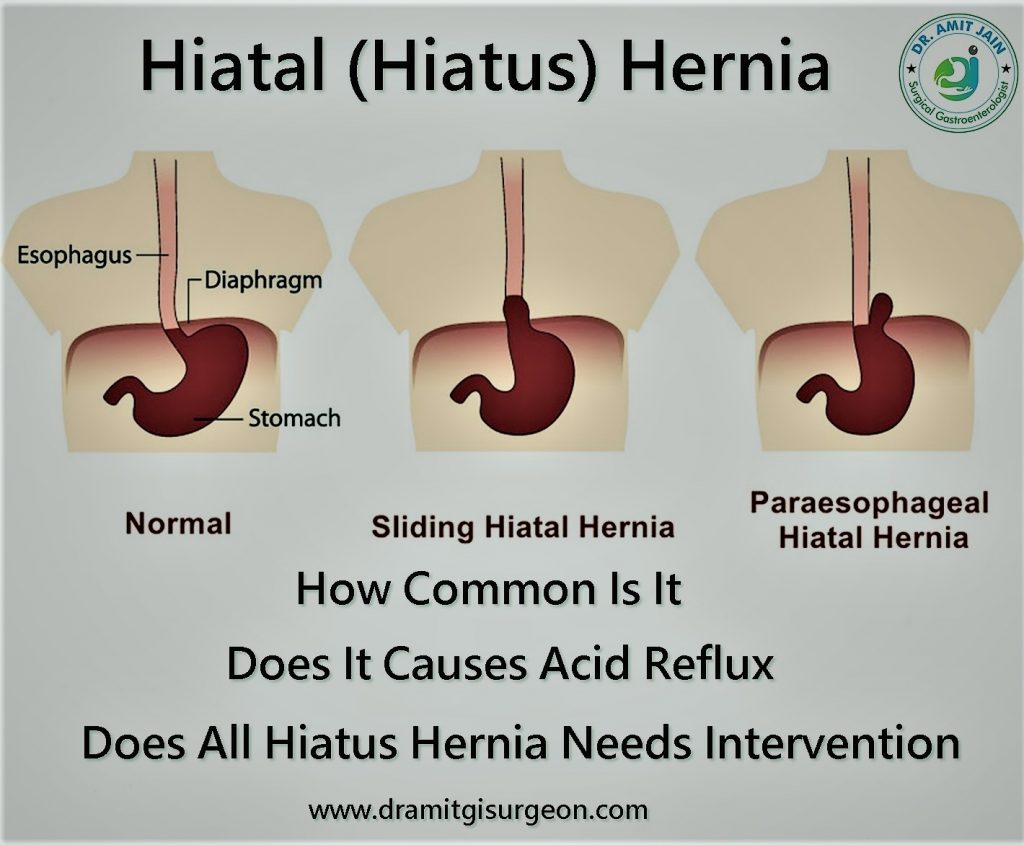
Hiatus Hernia
Diaphragam is a muscular wall which separates chest cavity from abdomen cavity. Hiatus is an opening in the diaphragam through which esophagus enters from thorax into the abdomen. A hiatus hernia occur when stomach most commonly or other abdomen organs enters into thorax through this openingTypes of Hiatus Hernia There are two types of hiatus hernia one is sliding and other is paraesophageal. In sliding hernia GE junction migrates into the thorax.In Paraesophageal hernia GE junction remains stable, stomach most commonly or other abdomen organs rolls into the thorax through side of Oesophagus
Symptoms: Most commonly patient present with long history of heartburn. Heartburn is defined as pressure sensation localized to epigastric and retrosternal area which does not radiate to back.As the disease become more severe patient complain of regurgitation of digested food. Dysphagia occur due to mechanical obstruction to food
Diagnosis: Upper GI Endoscopy is first step to rule out other disorders whose symptoms mimics with hiatus hernia. It also grades the esophagus injury severity due to acid reflux
Medical Treatment: Proton pump inhibitors and life style modification are first step in management of hiatus hernia
Surgical Management: Failed medical therapy, Large hiatus defect, Herniation of other abdomen organs are indications for surgery. The standard surgical procedure is reduction of hernia contents with repair of hiatus and fundoplication. It is Laparoscopic Surgery done with minimal incision
Achalasia Cardia
It is a surgical condition of the Oesophagus which causes impaired relaxation of lower esophageal sphincter muscle in response to swallowing. Patient complain of difficulty in swallowing and regurgitation. Upper GI endoscopy & manometery are diagnostic . Surgical procedure is Laparoscopic Hellers Myotomy.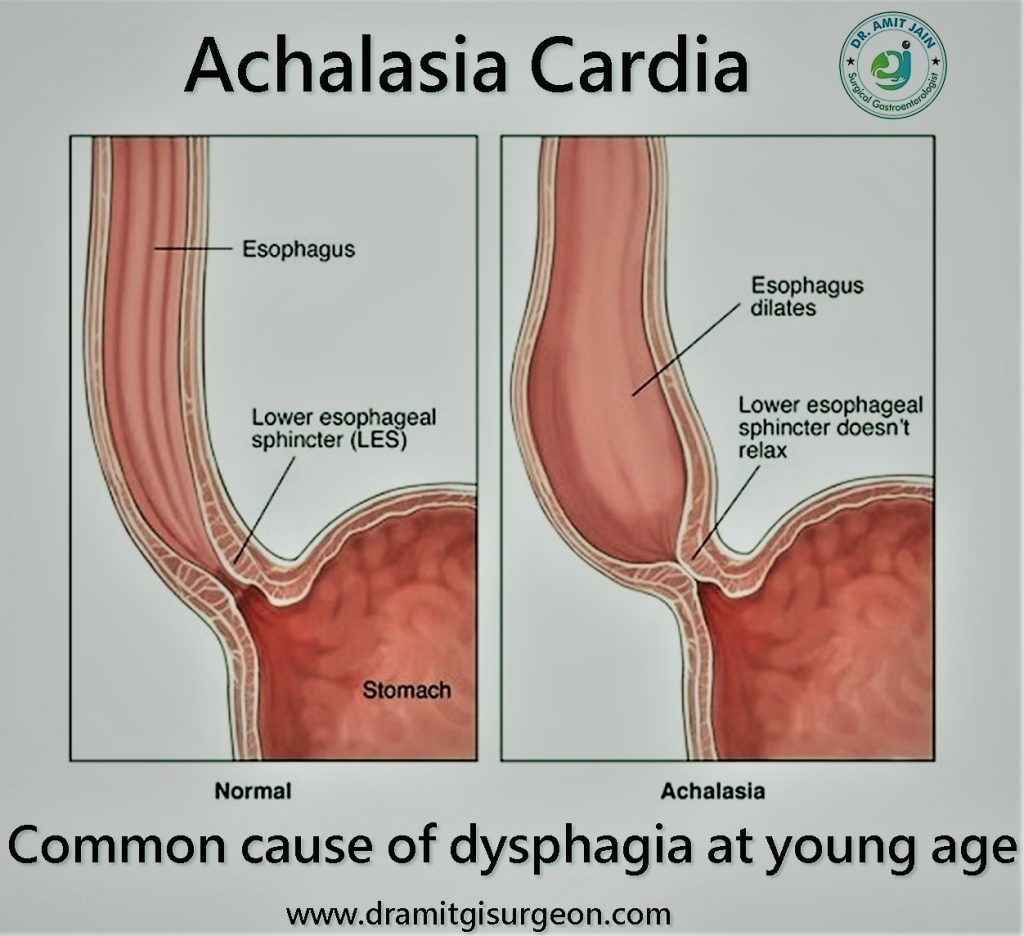
Corrosive Stricture
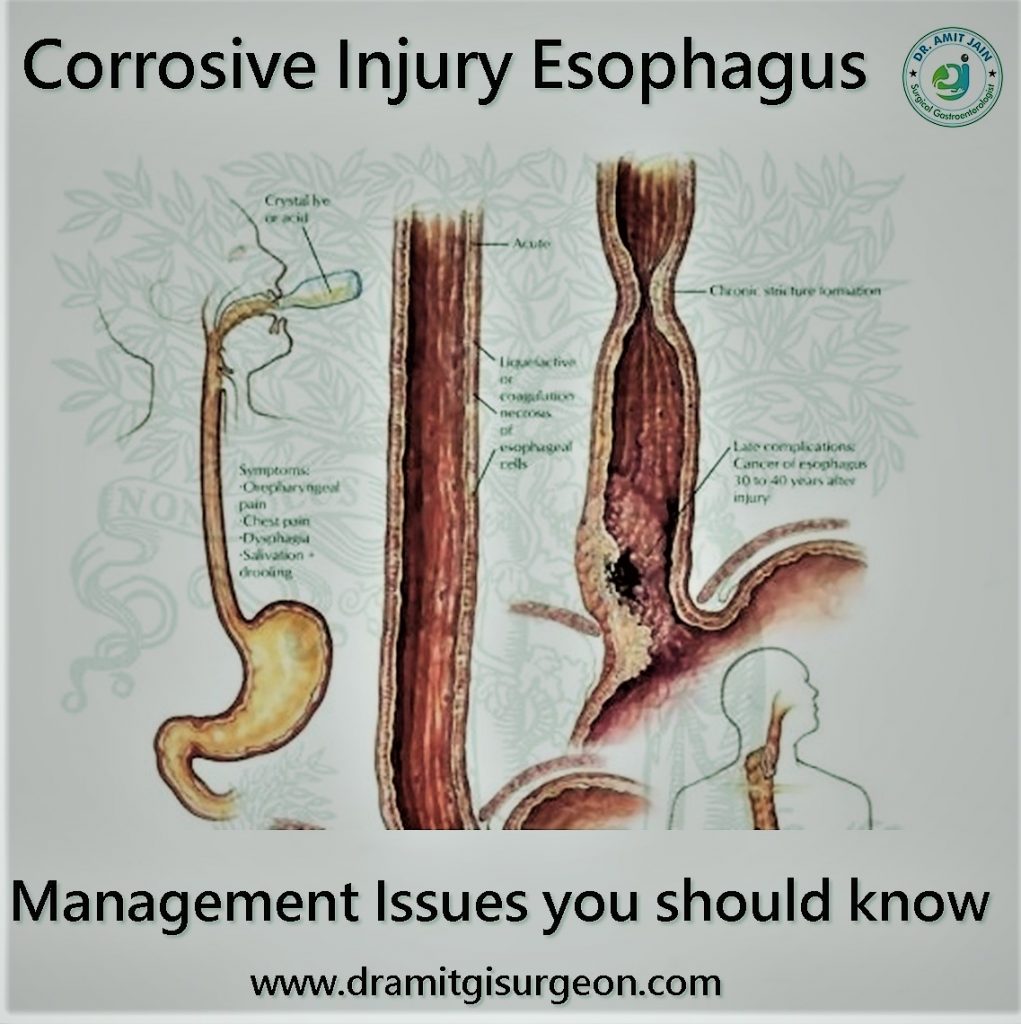
The incidence of corrosive esophagus injury has decreased. Mostly it is accidental and seen in children. Suicidal ingestion is seen in adults. It is of two types acid and alkali. Alkali because of its adhesive property causes esophagus injury.Acid ingestion causes mainly gastric injuryFirst-aid management: First step is ABC that is airway breathing circulation maintenance. If required tracheostomy should be done. Patient should be kept nil per mouth. No attempt should be done to put a ryles tube. Intravenous fluid should be started, Vitals should be monitored. No role of upper GI endoscopy at acute corrosive esophagus injury. X-ray Chest and abdomen should be done to look for pneumo-mediastinum and gas under diaphragam. If the patient condition remain stable should be allowed liquids one he is able to swallow saliva comfortably
Role of Upper GI Endoscopy: It is a controversial issue. Some suggest that it should be done while other does not recommed upper GI endoscopy in acute injury. Upper GI endoscopy helps in grading the sverity of injury. It does not change the management plan
Role of Surgery: If patient general condition is good, vitals are stable and there is difficulty in swallowing after 7-10 days of ingestion then feedding jejunostomy can be done to start nutrition If patient condition deteriorates CECT chest and abdomen should be done for esophagus and stomach or other organ perforation or necrosis. If present then damage control surgery should be done. No attempt to restore the bowel continuity should be done at this critical condition of the patient.

