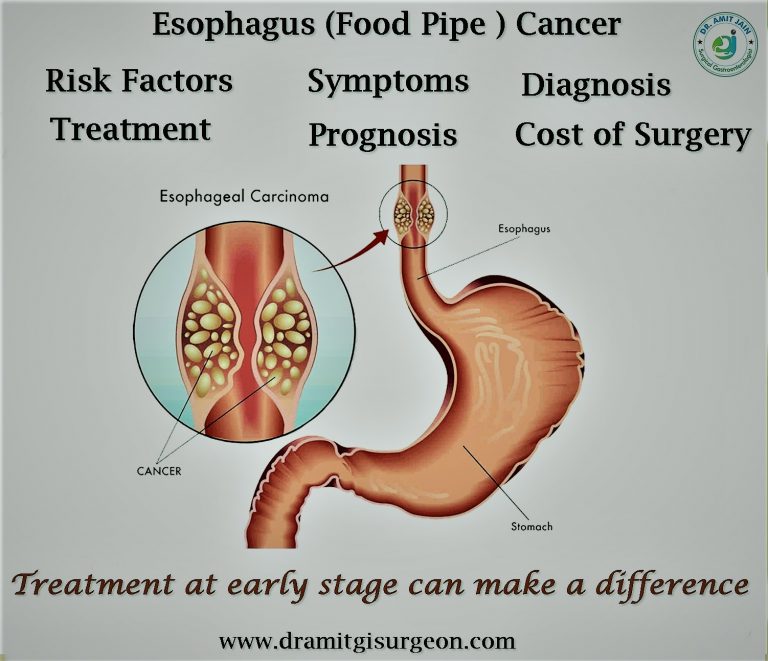

Cancer Oesophagus
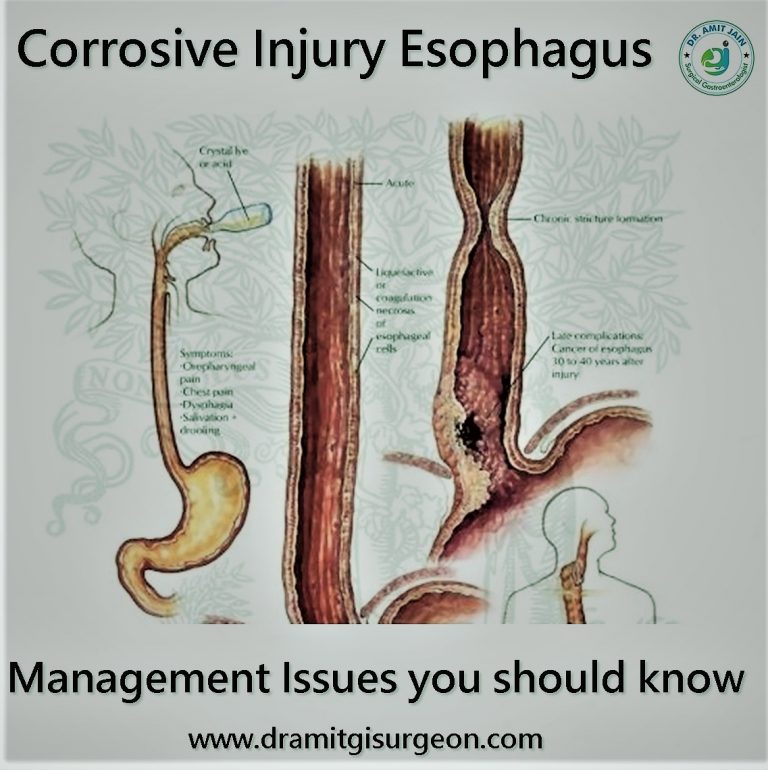
Smoking, alcohol intake, obesity and GERD are common Oesophagus cancer risk factor. Smoking and alcohol cause squamous cell carcinoma. Obesity and acid reflux are risk factors for adenocarcinoma. Healthy life style can prevent esophagus carcinoma The most common symptom is dysphagia. Initially it is for solid food and gradually to liquid also. Patient can have chest pain/regurgitation. Anorexia and weight loss are common. Advance carcinoma patients can have bony pain, abdomen distension due to ascites, respiratory distress due to pulmonary effusion.Diagnosis: Upper GI Endoscopy is done by gastroenterologist and is the investigation of choice. It will show growth or stricture in the esophagus. Biopsy will confirm the diagnosis. Most common type of esophagus carcinoma is adenocarcinoma located in the lower third of esophagus. Squamous cell carcinoma is other type and mainly found in the upper and middle third of esophagus
Investigations: CECT Chest and upper abdomen is done.CECT will show the growth in the esophagus, its relation with surrounding structures, any associated lymph nodes, and metastases. It helps in planning of Oesophagus carcinoma treatment. PET scan is done in selective patients who have bulky and long tumor and in high risk patients for surgery. The purpose is to identify distant metastases missed on CT scan
Treatment The recommended first line Esophagus Cancer Treatment is surgery if cancer is resectable. For locally advance tumor pre-operative chemo-radiotherapy is given.If patient respond to chemotherapy and tumor become resectable surgery is done. For metastatic disease endoscopic esophageal stent is placed for relief of dysphagia. If endoscopic stenting is not possible feeding jejunostomy is done surgically for nutrition