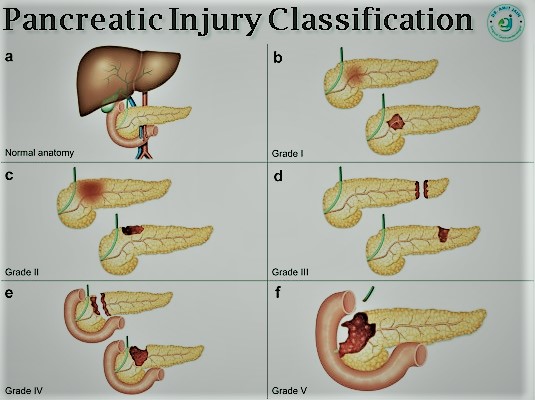
Pancreatic Injury
Traumatic injuries of the pancreas are uncommon and often difficult to diagnose owing to
subtle imaging findings, confounding multiorgan injuries, and nonspecific clinical signs.
Nonetheless, early diagnosis and treatment are critical, as delays increase morbidity and
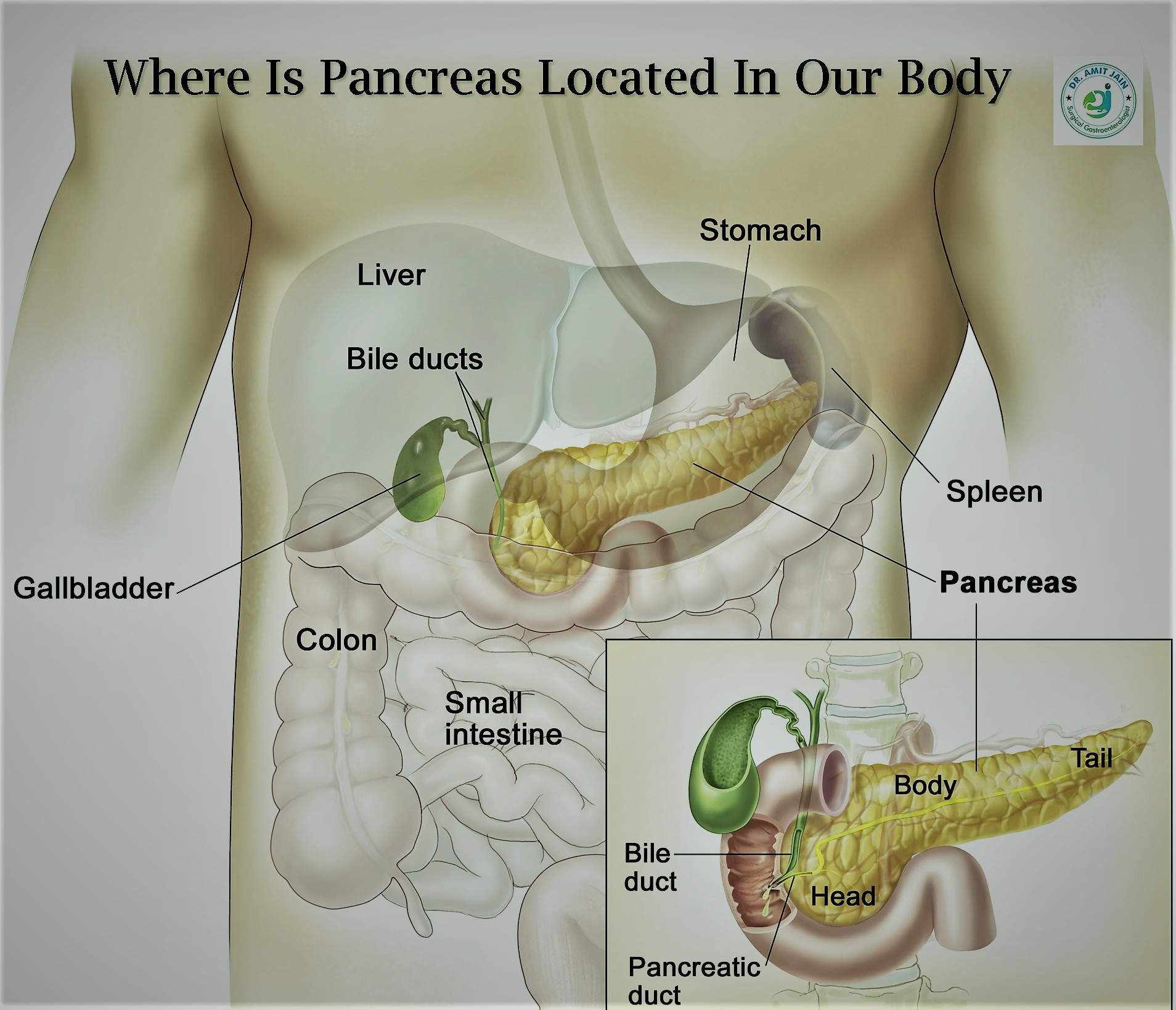
mortality. Imaging has a vital role in diagnosis and management. A high index of suspicion,
as well as knowledge of the anatomy, mechanism of injury, injury grade, and role of
available imaging modalities, is required for prompt accurate diagnosis. CT is the initial
imaging modality of choice, although the severity of injury can be underestimated and
assessment of the pancreatic duct is limited with this modality.
The time from
injury to definitive diagnosis and the treatment of potential pancreatic duct injury are the
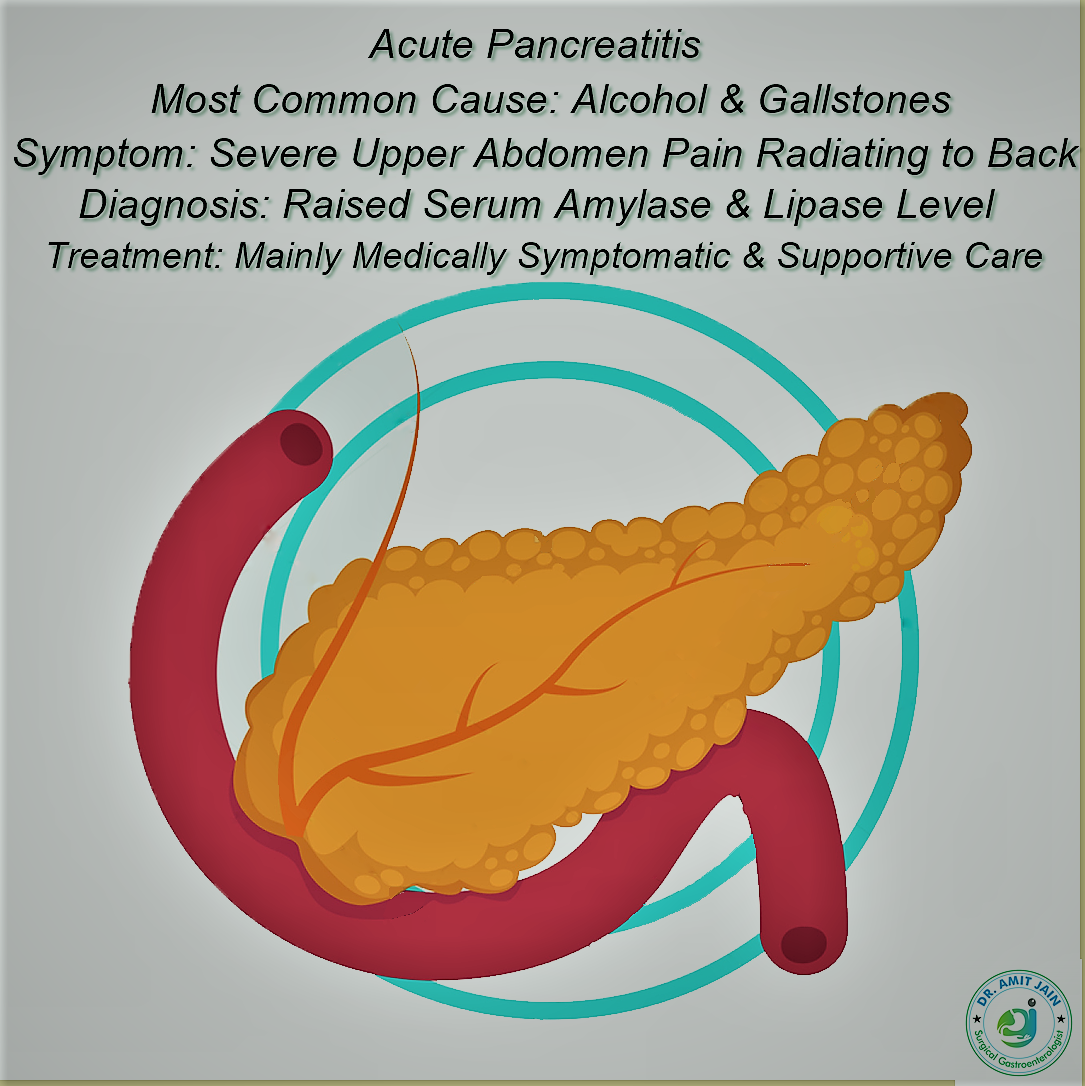
primary factors that determine outcome following pancreatic trauma. Disruption of the main
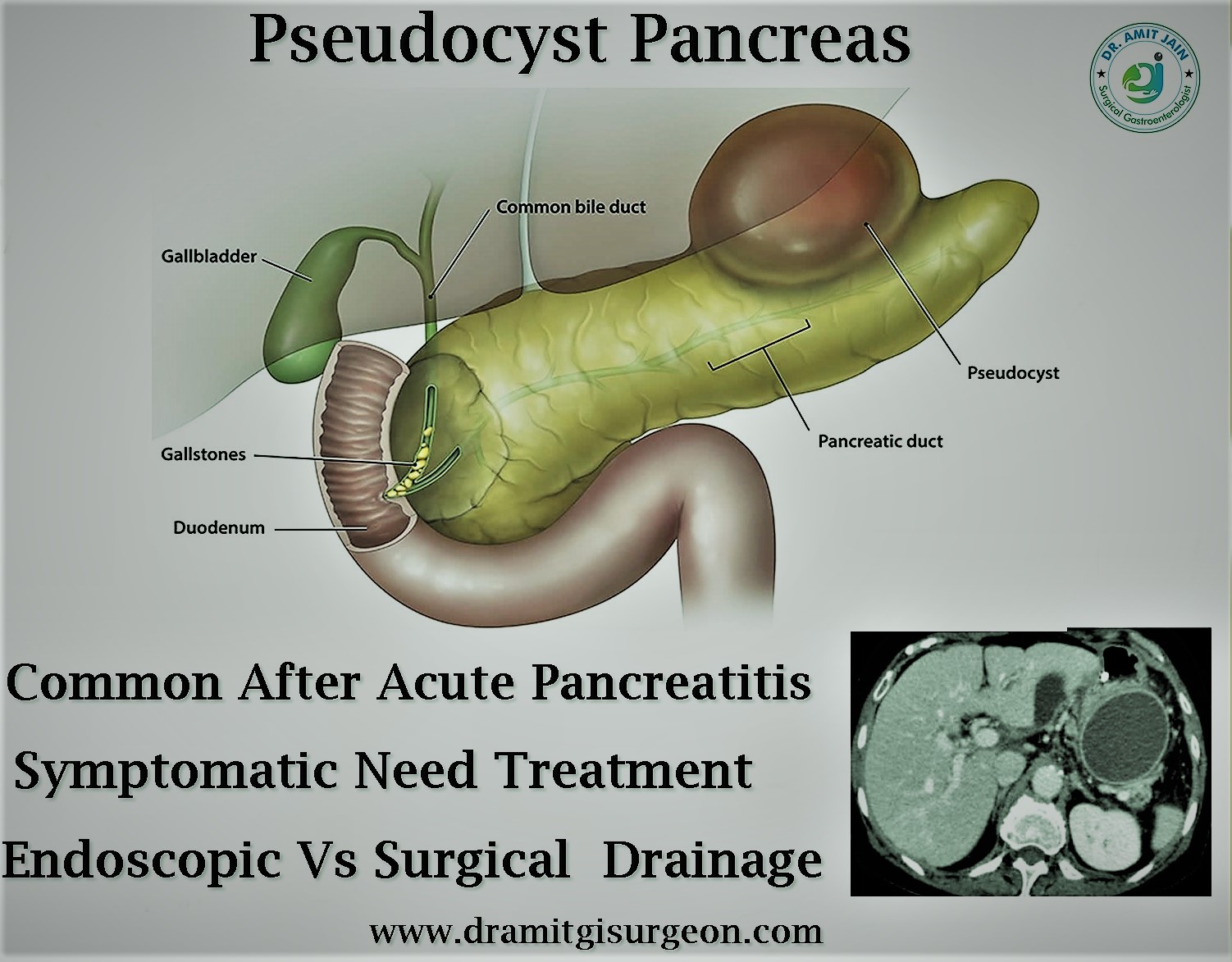
pancreatic duct (MPD) is associated with higher rates of complications, such as abscess,
fistula, and pseudoaneurysm, and is the primary cause of pancreatic injury–related
mortality. Although CT findings can suggest pancreatic duct disruption according to the
depth of parenchymal injury, MR cholangiopancreatography and endoscopic retrograde
cholangiopancreatography facilitate direct assessment of the MPD. Management of traumatic
pancreatic injury depends on multiple factors, including mechanism of injury, injury grade,
presence (or absence) of vascular injury, hemodynamic status of the patient, and associated
organ damage.