Pancreas: A Complete GI Surgery Guide
The pancreas is a crucial organ located deep in the abdomen behind the stomach. It plays a vital role in digestion, metabolism, and blood sugar regulation, making it essential for overall health. Although relatively small in size, pancreatic diseases — including pancreatitis, pancreatic cancer, cysts, and other disorders — can be serious and often require evaluation by a GI surgeon or hepatopancreatobiliary specialist.
What Is the Pancreas? (Anatomy & Function)
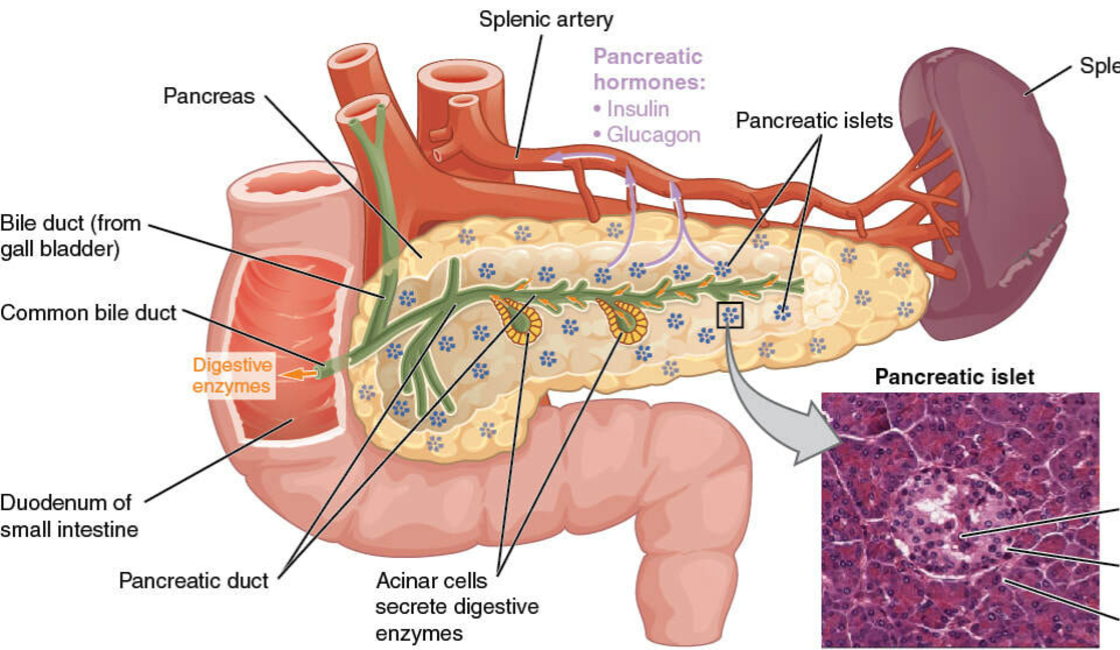
The pancreas is an elongated, flat gland that lies across the back of the upper abdomen behind the stomach. It is divided into the head, body, and tail, with each part playing a role in its complex functions.
The pancreas performs two primary functions:
Exocrine function: Produces digestive enzymes — such as amylase, lipase, and protease — that break down carbohydrates, fats, and proteins in the small intestine.
Endocrine function: Releases hormones like insulin and glucagon, which regulate blood sugar levels and help maintain metabolic balance throughout the body.
Without the pancreas functioning properly, both digestion and blood sugar regulation are affected, potentially leading to systemic problems such as malabsorption, diabetes, and nutritional deficiencies.
Common Pancreatic Disorders
Disorders of the pancreas vary in severity and may be acute or chronic. Some of the most important conditions include:
1. Pancreatitis (Pancreatic Inflammation)
Pancreatitis is inflammation of the pancreas that may be acute (sudden onset) or chronic (long-term). Acute pancreatitis often presents with severe abdominal pain, nausea, vomiting, fever, and swelling of the pancreas. If not treated promptly, it can lead to complications such as necrosis (tissue death), infections, or organ failure.
Chronic pancreatitis is a progressive condition that can cause ongoing pain, malabsorption, and eventually diabetes due to loss of endocrine function. Common triggers include gallstones, alcohol use, high triglyceride levels, and genetic conditions.
2. Pancreatic Cancer
Pancreatic cancer arises when abnormal cells grow within pancreatic tissue. It often shows few symptoms in early stages, which makes early detection difficult. Symptoms may include unexplained weight loss, upper abdominal pain that radiates to the back, jaundice (yellowing of the skin or eyes), and changes in stool.
Because the pancreas sits deep within the abdomen, tumors are often not detected until they are advanced. Surgical treatment (such as pancreatic resection) and multidisciplinary oncology care are the mainstays of management.
3. Pancreatic Cysts and Other Lesions
Pancreatic cysts are fluid-filled sacs that can be benign or precancerous. Some types, like mucinous cystic neoplasms, have a risk of turning into cancer and may require monitoring or surgical removal.
4. Endocrine Disorders (Diabetes)
Since the pancreas produces insulin and glucagon, damage to its endocrine cells — as in chronic pancreatitis or autoimmune conditions — can lead to type 3c diabetes or impair blood sugar control.
Symptoms of Pancreatic Problems
Symptoms vary with the type and severity of disease but commonly include:
Severe upper abdominal pain that may radiate to the back
Nausea and vomiting
Unexplained weight loss
Fatty or foul-smelling stools (steatorrhea)
Jaundice (yellowing of skin/eyes)
Uncontrolled blood sugar levels
Fatigue and loss of appetite
Because these symptoms overlap with other conditions, proper medical evaluation is necessary for accurate diagnosis and treatment.
Diagnosis: How Pancreatic Diseases Are Evaluated
Doctors use multiple tools to diagnose pancreatic problems:
Blood tests: To check pancreatic enzymes (amylase, lipase), liver function, and blood glucose.
Imaging studies:
Ultrasound and CT scans reveal structural abnormalities or inflammation.
MRI and MRCP (Magnetic Resonance Cholangiopancreatography) provide detailed imaging of ducts and cysts.
Endoscopic ultrasound (EUS): Combines endoscopy and ultrasound to assess tumors and cysts closely.
Biopsy: Tissue sampling may be done when malignancy is suspected.
Accurate diagnosis guides the choice between medical management, interventional procedures, or surgery.
Treatment Options for Pancreatic Conditions
1. Medical and Conservative Management
Mild or early pancreatic inflammation may be treated with fasting (to rest the pancreas), intravenous fluids, pain control, and treatment of underlying causes such as gallstones or high triglycerides.
2. Endoscopic and Interventional Procedures
For certain conditions like pancreatic duct stones, ductal strictures, or cyst drainage, endoscopic approaches such as ERCP (Endoscopic Retrograde Cholangiopancreatography) may be used.
3. Surgical Treatment
Surgery plays a crucial role in managing severe or recurrent pancreatic problems:
Pancreatic Resection: This includes procedures like Whipple surgery(pancreaticoduodenectomy) for tumors in the head of the pancreas, or distal pancreatectomy for tumors in the body/tail of the pancreas. These complex operations are typically performed by experienced GI or hepatopancreatobiliary surgeons.
Surgery for Chronic Pancreatitis: In resistant cases with persistent pain or complications, procedures such as lateral pancreaticojejunostomy may be recommended.
Pancreas Transplantation: In select patients with diabetes and pancreatic failure, pancreas or islet cell transplantation may be considered.
Modern surgical approaches often incorporate laparoscopic and minimally invasive techniques, which may offer faster recovery and reduced pain.
Recovery and Long-Term Care
Patients undergoing pancreatic surgery or treatment of chronic disease require:
Careful monitoring of nutrition and enzyme replacement
Blood sugar management
Regular imaging and follow-up
Lifestyle adjustments such as avoiding alcohol and maintaining a balanced diet
Long-term outcomes depend on the specific disease and overall health status at the time of diagnosis.
Preventive Strategies & Healthy Practices
Maintaining pancreatic health includes:
Eating a balanced, low-fat diet
Limiting alcohol consumption and smoking
Controlling blood sugar and triglyceride levels
Regular health screenings especially if there is a family history of pancreatic disease
Early detection improves outcomes, particularly for conditions like pancreatic cancer where symptoms may appear late.
Dr. Amit Jain – Laparoscopic & Robotic GI Surgeon in Greater Noida
Dr. Amit Jain is a highly experienced and renowned GI, Laparoscopic & Robotic Surgeon with specialized expertise in liver, pancreas, biliary tract, and gastrointestinal cancers. He is recognized as one of the best GI surgeons in Greater Noida and India, offering advanced surgical care for complex pancreatic and hepatobiliary conditions.
Learn more or book your consultation with Dr. Amit Jain: https://dramitgisurgeon.com
Conclusion
The pancreas is indispensable to digestion and hormone regulation. Diseases affecting this organ — from pancreatitis to pancreatic cancer — require timely and accurate diagnosis and management. With advances in medical imaging, minimally invasive treatment, and expert GI surgery, many pancreatic conditions can be effectively treated. Consulting a qualified GI surgeon or hepatopancreatobiliary specialist ensures that each patient receives personalized care tailored to the severity and type of pancreatic disease.